Who We Are
Montgomery Hospice was the first independent hospice licensed in Maryland.

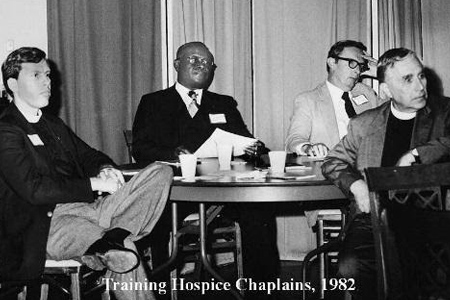
1981
Volunteers founded our core service, Hospice at Home, in the basement of a church in Chevy Chase in 1981.

1999
Casey House opened in 1999, and is the only medical facility in Montgomery County exclusively designed and built to comfort the dying. Patients of Montgomery Hospice and Prince George’s Hospice go to Casey House to receive General Inpatient Care.

2019
In August of 2019, Montgomery Hospice’s services expanded into Prince George’s County – forming Montgomery Hospice and Prince George’s Hospice.

Current
Montgomery Hospice and Prince George’s Hospice has grown from serving seven patients in 1981 as Montgomery Hospice, to more than 2,000 patients now across Montgomery and Prince George’s Counties, with 5,700 family and community members receiving bereavement support annually.
STAFF & BOARD
We are nurses, doctors, and hospice aides. We are social workers and chaplains. We are accountants and fundraisers. Together we work to provide compassionate comfort care and to support the grieving members of our community.
Staff Leadership

 Ann Mitchell has been in hospice management since 1981 when a year later, she lobbied for passage of the Medicare Hospice Benefit. Prior to coming to Montgomery Hospice in 1998, she worked for non-profit hospices in Massachusetts and South Carolina. In the late 1980’s she was instrumental in the development of an AIDS inpatient hospice in the Boston area.
Ann Mitchell has been in hospice management since 1981 when a year later, she lobbied for passage of the Medicare Hospice Benefit. Prior to coming to Montgomery Hospice in 1998, she worked for non-profit hospices in Massachusetts and South Carolina. In the late 1980’s she was instrumental in the development of an AIDS inpatient hospice in the Boston area.
Ann is a Board Director of the Hospice Alliance, a collaboration of regional hospices that works, through Alliance Kids, to enhance quality pediatric hospice service. Ann also is the Vice President of the Retirement Services Board of Directors of Maplewood Park Place, a continuing care retirement community located in Bethesda.
Ann majored in economics at Smith College, and in 1981 earned her Masters in Public Health from Yale University’s School of Public Health. She also took courses at the Yale School of Management to satisfy the requirements for her concentration in hospital administration. In the mid-1990’s Ann was the principal investigator of a study, published as a letter in JAMA (Journal of the American Medical Association), on the economics of hospice care.
Ann is a member of the Leadership Montgomery Class of 2015 and a trustee emeritus of Smith College.
 Dr. David Schrier serves as the organization’s Chief Medical Officer/Medical Director. Dr. Schrier received his medical degree from the University of Colorado Health Sciences Center, followed by a fellowship in Hematology-Oncology. He received board-certification in Medical Oncology, establishing a successful practice with a mission to deliver comprehensive medical and emotional care to patients and their families, with emphasis on the whole patient. As a medical oncologist, his involvement with helping patients and family members navigate end of life issues led him to become a Hospice Medical Director, a position he has held since 2007. Dr. Schrier has extensive experience with non-medical aspects of practice – including staffing, scheduling, marketing, advertising, education, and community involvement. Dr. Schrier has a lifelong passion for animals (especially dogs), art, philanthropy, equestrian competition, physical fitness/nutrition, gardening, and community service.
Dr. David Schrier serves as the organization’s Chief Medical Officer/Medical Director. Dr. Schrier received his medical degree from the University of Colorado Health Sciences Center, followed by a fellowship in Hematology-Oncology. He received board-certification in Medical Oncology, establishing a successful practice with a mission to deliver comprehensive medical and emotional care to patients and their families, with emphasis on the whole patient. As a medical oncologist, his involvement with helping patients and family members navigate end of life issues led him to become a Hospice Medical Director, a position he has held since 2007. Dr. Schrier has extensive experience with non-medical aspects of practice – including staffing, scheduling, marketing, advertising, education, and community involvement. Dr. Schrier has a lifelong passion for animals (especially dogs), art, philanthropy, equestrian competition, physical fitness/nutrition, gardening, and community service.

Jennifer Plude started at Montgomery Hospice, Inc. in 2016 and currently holds the position of Chief Clinical Officer. During her seven years at Montgomery Hospice, Inc., she has worked in various capacities as a Clinical Manager and Afterhours Manager. Jennifer has been a professional Registered Nurse for over 30 years and has over 20 years of leadership experience in both the hospital and hospice settings. Jennifer’s nursing experience as a pediatric oncology nurse is where she began her journey to end-of-life care. She serves as a Board Director for the Hospice & Palliative Care Network of Maryland and is a Certified Hospice and Palliative Nurse (CHPN).
 Marlene Bradford has nearly 30 years of experience raising funds for healthcare and education nonprofit organizations in the Washington metropolitan area. She has a proven track record in the management of fundraising programs, including major gift stewardship and solicitation, corporate sponsorships, event planning, grant writing, and board development. In her role, she is also responsible for the communications and the education and outreach initiatives of the organization. In addition, Marlene oversees the organization’s Diversity Equity and Inclusion initiatives.
Marlene Bradford has nearly 30 years of experience raising funds for healthcare and education nonprofit organizations in the Washington metropolitan area. She has a proven track record in the management of fundraising programs, including major gift stewardship and solicitation, corporate sponsorships, event planning, grant writing, and board development. In her role, she is also responsible for the communications and the education and outreach initiatives of the organization. In addition, Marlene oversees the organization’s Diversity Equity and Inclusion initiatives.
Marlene is a graduate of the University of Toledo, Leadership Montgomery’s CORE Class (2018), and Racial Equity Action Leadership Inclusion Program (2020). She is also a member of the Development Committee at Generation Hope.
 Cornelia Stronge is a Registered Nurse with over twenty-five years of nursing experience, thirteen of which has been in management and leadership. She obtained her BSN degree from City University in London, and in 2021 she obtained a master’s in healthcare administration (MHA) degree from the University of Maryland. She is a Certified Hospice and Palliative Nurse (CHPN) since 2009.
Cornelia Stronge is a Registered Nurse with over twenty-five years of nursing experience, thirteen of which has been in management and leadership. She obtained her BSN degree from City University in London, and in 2021 she obtained a master’s in healthcare administration (MHA) degree from the University of Maryland. She is a Certified Hospice and Palliative Nurse (CHPN) since 2009.
During her fifteen years at Montgomery Hospice and Prince George’s Hospice, she has worked in various capacities as a Nurse Case Manager, Clinical Manager, and VP of Strategic Development. She is committed to empowering the staff to provide quality hospice care that not only meets but surpasses Federal and regulatory standards.
Physicians and Nurse Practitioners
Chief Medical Officer / Medical Director
 Dr. David Schrier received his medical degree from the University of Colorado Health Sciences Center, followed by a fellowship in Hematology-Oncology. He received board-certification in Medical Oncology, establishing a successful practice with a mission to deliver comprehensive medical and emotional care to patients and their families, with emphasis on the whole patient. As a medical oncologist, his involvement with helping patients and family members navigate end of life issues led him to become a Hospice Medical Director, a position he has held since 2007. Dr. Schrier has extensive experience with non-medical aspects of practice – including staffing, scheduling, marketing, advertising, education, and community involvement. Dr. Schrier has a lifelong passion for animals (especially dogs), art, philanthropy, equestrian competition, physical fitness/nutrition, gardening, and community service.
Dr. David Schrier received his medical degree from the University of Colorado Health Sciences Center, followed by a fellowship in Hematology-Oncology. He received board-certification in Medical Oncology, establishing a successful practice with a mission to deliver comprehensive medical and emotional care to patients and their families, with emphasis on the whole patient. As a medical oncologist, his involvement with helping patients and family members navigate end of life issues led him to become a Hospice Medical Director, a position he has held since 2007. Dr. Schrier has extensive experience with non-medical aspects of practice – including staffing, scheduling, marketing, advertising, education, and community involvement. Dr. Schrier has a lifelong passion for animals (especially dogs), art, philanthropy, equestrian competition, physical fitness/nutrition, gardening, and community service.
Physicians
Montgomery Kids Physician
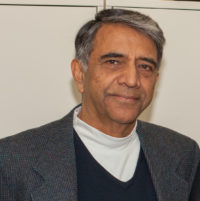 Dr. Aziz, who is board certified in pediatrics, medical management, and hospice and palliative medicine, has talked to patients and their caregivers about end-of-life decisions over a thousand times in the last twenty years. After graduating from King Edward Medical College in Lahore, Pakistan, he trained in pediatrics at the University of Maryland, Saint Agnes, and Mercy hospitals. He has been on the clinical faculty of the University of Maryland and Johns Hopkins, along with multiple local hospitals in the Baltimore metropolitan area. He served as Assistant Chair of Pediatrics at Saint Agnes hospital, then Chair of Pediatrics and the Ethics Committee, as well as the VPMA at Medstar Harbor Hospital, all in Baltimore, Maryland. Dr. Aziz was instrumental in helping start the pediatric hospice services at Hospice of Chesapeake in Maryland and the Palliative Care Program at Laurel Regional Hospital in Maryland. He continues to chair multiple ethics committees, as well as serve on hospice/palliative care teams at local hospitals and at Montgomery Hospice in Rockville, Maryland, helping take care of children and adults. He is also actively involved in the education of the public and medical personnel.
Dr. Aziz, who is board certified in pediatrics, medical management, and hospice and palliative medicine, has talked to patients and their caregivers about end-of-life decisions over a thousand times in the last twenty years. After graduating from King Edward Medical College in Lahore, Pakistan, he trained in pediatrics at the University of Maryland, Saint Agnes, and Mercy hospitals. He has been on the clinical faculty of the University of Maryland and Johns Hopkins, along with multiple local hospitals in the Baltimore metropolitan area. He served as Assistant Chair of Pediatrics at Saint Agnes hospital, then Chair of Pediatrics and the Ethics Committee, as well as the VPMA at Medstar Harbor Hospital, all in Baltimore, Maryland. Dr. Aziz was instrumental in helping start the pediatric hospice services at Hospice of Chesapeake in Maryland and the Palliative Care Program at Laurel Regional Hospital in Maryland. He continues to chair multiple ethics committees, as well as serve on hospice/palliative care teams at local hospitals and at Montgomery Hospice in Rockville, Maryland, helping take care of children and adults. He is also actively involved in the education of the public and medical personnel.
Team Physician
 Dr. Geoffrey Coleman attended the Georgia Institute of Technology (Mechanical Engineering) and Temple University School of Medicine in Philadelphia. His first residency training was in emergency medicine, an experience which persuaded him to pursue a career that allowed more hands-on patient contact. He decided to switch to family medicine and earned his board certification in this specialty. Dr. Coleman spent his first year of practice in Kenya and Sierra Leone, Africa. On his return to the United States he provided primary medical care for nine years on the Menominee Indian Reservation in Wisconsin. Moving east to be near family, he established a community health center in Montross, Virginia, providing primary and preventive healthcare, with regular house calls to patients. He continued his passion for direct patient care, and for home visits, when he moved into hospice work by starting a practice focusing on home visits and palliative care in 2004. He served as its medical director. Since 2007 Dr. Coleman has practiced hospice and palliative medicine exclusively. Dr. Coleman is certified in Hospice & Palliative Medicine and in Family Medicine.
Dr. Geoffrey Coleman attended the Georgia Institute of Technology (Mechanical Engineering) and Temple University School of Medicine in Philadelphia. His first residency training was in emergency medicine, an experience which persuaded him to pursue a career that allowed more hands-on patient contact. He decided to switch to family medicine and earned his board certification in this specialty. Dr. Coleman spent his first year of practice in Kenya and Sierra Leone, Africa. On his return to the United States he provided primary medical care for nine years on the Menominee Indian Reservation in Wisconsin. Moving east to be near family, he established a community health center in Montross, Virginia, providing primary and preventive healthcare, with regular house calls to patients. He continued his passion for direct patient care, and for home visits, when he moved into hospice work by starting a practice focusing on home visits and palliative care in 2004. He served as its medical director. Since 2007 Dr. Coleman has practiced hospice and palliative medicine exclusively. Dr. Coleman is certified in Hospice & Palliative Medicine and in Family Medicine.
Casey House Physician
 Dr. Jasmine Gatti is a palliative and geriatric MD educated at Johns Hopkins University, Georgetown University School of Medicine, and University of Maryland Medical Systems. Raised in the DMV, she served for over 25 years in clinical practices including her own. She was a GWU adjunct professor in the Department of Geriatrics at the Veteran’s Administration Heath Care of DC, a director of Inpatient Hospice of Holy Cross Home Care, and a director of Home Visits at Hebrew Home of Greater Washington, DC. She also has a successful career at the FDA and is certified in palliative medicine, geriatrics, and family medicine. As a family physician, she believes in a holistic, compassionate approach to care involving the physical, spiritual, emotional aspects and the support of others.
Dr. Jasmine Gatti is a palliative and geriatric MD educated at Johns Hopkins University, Georgetown University School of Medicine, and University of Maryland Medical Systems. Raised in the DMV, she served for over 25 years in clinical practices including her own. She was a GWU adjunct professor in the Department of Geriatrics at the Veteran’s Administration Heath Care of DC, a director of Inpatient Hospice of Holy Cross Home Care, and a director of Home Visits at Hebrew Home of Greater Washington, DC. She also has a successful career at the FDA and is certified in palliative medicine, geriatrics, and family medicine. As a family physician, she believes in a holistic, compassionate approach to care involving the physical, spiritual, emotional aspects and the support of others.
Casey House Physician
 Dr. Ghosh has worked at Montgomery Hospice and Prince George’s Hospice since 2018. She finished her residency in Internal Medicine at Washington Hospital Center, and her fellowship in Palliative Care and Hospice at the National Institutes of Health. She has experience with both palliative care and end-of-life hospice patients.
Dr. Ghosh has worked at Montgomery Hospice and Prince George’s Hospice since 2018. She finished her residency in Internal Medicine at Washington Hospital Center, and her fellowship in Palliative Care and Hospice at the National Institutes of Health. She has experience with both palliative care and end-of-life hospice patients.
Casey House Physician
 Dr. Ruthann Giusti attended the University of Massachusetts in Amherst, MA, where she completed her undergraduate degree in Zoology and Masters in Public Health. She attended the University of Massachusetts Medical School in Worcester, MA, residency in Internal Medicine at Albany Medical Center in Albany, NY, and an Oncology Fellowship at the National Cancer Institute. After working for many years at the Food and Drug Administration helping to develop new cancer drugs, she decided to return to patient care and did a fellowship in Hospice and Palliative Medicine at the National Institutes of Health, where she continues to practice part-time. She is pleased to work with the wonderful staff and patients at Casey House. Dr. Giusti is Boarded in Internal Medicine and Hospice and Palliative Care and Board Eligible in Medical Oncology. When not working, Dr. Giusti loves to garden, read, spend time with her two adult daughters and extended family, and cook Italian food.
Dr. Ruthann Giusti attended the University of Massachusetts in Amherst, MA, where she completed her undergraduate degree in Zoology and Masters in Public Health. She attended the University of Massachusetts Medical School in Worcester, MA, residency in Internal Medicine at Albany Medical Center in Albany, NY, and an Oncology Fellowship at the National Cancer Institute. After working for many years at the Food and Drug Administration helping to develop new cancer drugs, she decided to return to patient care and did a fellowship in Hospice and Palliative Medicine at the National Institutes of Health, where she continues to practice part-time. She is pleased to work with the wonderful staff and patients at Casey House. Dr. Giusti is Boarded in Internal Medicine and Hospice and Palliative Care and Board Eligible in Medical Oncology. When not working, Dr. Giusti loves to garden, read, spend time with her two adult daughters and extended family, and cook Italian food.
Casey House Physician
 Dr. Joseph received her medical degree from JSS Medical College in Karnataka, India. She did her residency in family practice at The Toledo Hospital, Toledo Ohio. Dr. Joseph did a Geriatric Medicine Fellowship in George Washington University, Washington DC. Her work experience includes working as a geriatrician at Ascension Providence, Washington DC, since 2004, as medical director at Center for Geriatric Medicine and Carroll Manor Nursing Home and Rehabilitation at Washington DC, and as a Montgomery Hospice inpatient physician. She is an assistant professor at George Washington Medical School. Dr. Joseph is Board Certified in Family Practice, Geriatric Medicine, Hospice and Palliative Care, and Wound Care. She has been listed as a Washingtonian Top Doctor in 2016 and 2017 and describes herself as “passionate about geriatric and palliative care.”
Dr. Joseph received her medical degree from JSS Medical College in Karnataka, India. She did her residency in family practice at The Toledo Hospital, Toledo Ohio. Dr. Joseph did a Geriatric Medicine Fellowship in George Washington University, Washington DC. Her work experience includes working as a geriatrician at Ascension Providence, Washington DC, since 2004, as medical director at Center for Geriatric Medicine and Carroll Manor Nursing Home and Rehabilitation at Washington DC, and as a Montgomery Hospice inpatient physician. She is an assistant professor at George Washington Medical School. Dr. Joseph is Board Certified in Family Practice, Geriatric Medicine, Hospice and Palliative Care, and Wound Care. She has been listed as a Washingtonian Top Doctor in 2016 and 2017 and describes herself as “passionate about geriatric and palliative care.”
Hospice Physician
 Dr. Ann Lichtenstein received her Doctorate of Osteopathic Medicine from New York College of Osteopathic Medicine in Old Westbury, New York. She completed her Internship at Maimonides Medical Center in Brooklyn, New York. Motivated by her passion for movement and exercise she specialized in Physical Medicine and Rehabilitation during her Residency at the Icahn School of Medicine at Mount Sinai in New York, New York. Her interest in pain and symptom management led her to a Fellowship in Hospice and Palliative Medicine at the National Institutes of Health. Dr. Lichtenstein has contributed several chapters to textbooks on Rehabilitation and Palliative Medicine and also has published a number of research articles. She continues to be involved in medical training with Hospice and Palliative Medicine Fellows from NIH and Children’s Hospital Center. She is board certified in Physical Medicine and Rehabilitation and board eligible in Hospice & Palliative Medicine.
Dr. Ann Lichtenstein received her Doctorate of Osteopathic Medicine from New York College of Osteopathic Medicine in Old Westbury, New York. She completed her Internship at Maimonides Medical Center in Brooklyn, New York. Motivated by her passion for movement and exercise she specialized in Physical Medicine and Rehabilitation during her Residency at the Icahn School of Medicine at Mount Sinai in New York, New York. Her interest in pain and symptom management led her to a Fellowship in Hospice and Palliative Medicine at the National Institutes of Health. Dr. Lichtenstein has contributed several chapters to textbooks on Rehabilitation and Palliative Medicine and also has published a number of research articles. She continues to be involved in medical training with Hospice and Palliative Medicine Fellows from NIH and Children’s Hospital Center. She is board certified in Physical Medicine and Rehabilitation and board eligible in Hospice & Palliative Medicine.
Team Physician
 Dr. Angela Lipshutz received her medical degree from the University of California, San Francisco (UCSF) School of Medicine and master’s degree in public health from the Johns Hopkins University Bloomberg School of Public Health. She completed an internship in Internal Medicine at Stanford University, followed by residency in Anesthesiology and fellowship in Critical Care Medicine at UCSF. She spent several years on the faculty at UCSF as an anesthesiologist and intensivist, during which she developed a passion for symptom management, end of life care, and patient and family engagement. To develop further expertise in these areas, Dr. Lipshutz completed a fellowship in Hospice and Palliative Medicine at the National Institutes of Health. She maintains an affiliation with the Pain and Palliative Care Service at the NIH, where she focuses on quality improvement, medical simulation, and trainee wellbeing. Dr. Lipshutz is board certified in Anesthesiology, Critical Care Medicine, and Hospice and Palliative Medicine.
Dr. Angela Lipshutz received her medical degree from the University of California, San Francisco (UCSF) School of Medicine and master’s degree in public health from the Johns Hopkins University Bloomberg School of Public Health. She completed an internship in Internal Medicine at Stanford University, followed by residency in Anesthesiology and fellowship in Critical Care Medicine at UCSF. She spent several years on the faculty at UCSF as an anesthesiologist and intensivist, during which she developed a passion for symptom management, end of life care, and patient and family engagement. To develop further expertise in these areas, Dr. Lipshutz completed a fellowship in Hospice and Palliative Medicine at the National Institutes of Health. She maintains an affiliation with the Pain and Palliative Care Service at the NIH, where she focuses on quality improvement, medical simulation, and trainee wellbeing. Dr. Lipshutz is board certified in Anesthesiology, Critical Care Medicine, and Hospice and Palliative Medicine.
Casey House Physician
 Dr. Kathleen McCabe attended Barnard College in New York City and the Philadelphia College of Osteopathic Medicine in Philadelphia. She completed an Internal Medicine internship at Elmhurst Hospital Center in Queens, New York and a residency in Physical Medicine and Rehabilitation at Mount Sinai in New York City. She then completed a fellowship in Hospice and Palliative Medicine at George Washington University. During that time she developed a passion for in-patient hospice and was pleased to have the opportunity to join the team at Casey House. Dr. McCabe is board eligible in Hospice & Palliative Medicine.
Dr. Kathleen McCabe attended Barnard College in New York City and the Philadelphia College of Osteopathic Medicine in Philadelphia. She completed an Internal Medicine internship at Elmhurst Hospital Center in Queens, New York and a residency in Physical Medicine and Rehabilitation at Mount Sinai in New York City. She then completed a fellowship in Hospice and Palliative Medicine at George Washington University. During that time she developed a passion for in-patient hospice and was pleased to have the opportunity to join the team at Casey House. Dr. McCabe is board eligible in Hospice & Palliative Medicine.
Chief Medical Officer/Medical Director
 Dr. David Schrier received his medical degree from the University of Colorado Health Sciences Center, followed by a fellowship in Hematology-Oncology. He received board-certification in Medical Oncology, establishing a successful practice with a mission to deliver comprehensive medical and emotional care to patients and their families, with emphasis on the whole patient. As a medical oncologist, his involvement with helping patients and family members navigate end of life issues led him to become a Hospice Medical Director, a position he has held since 2007. Dr. Schrier has extensive experience with non-medical aspects of practice – including staffing, scheduling, marketing, advertising, education, and community involvement. Dr. Schrier has a lifelong passion for animals (especially dogs), art, philanthropy, equestrian competition, physical fitness/nutrition, gardening, and community service.
Dr. David Schrier received his medical degree from the University of Colorado Health Sciences Center, followed by a fellowship in Hematology-Oncology. He received board-certification in Medical Oncology, establishing a successful practice with a mission to deliver comprehensive medical and emotional care to patients and their families, with emphasis on the whole patient. As a medical oncologist, his involvement with helping patients and family members navigate end of life issues led him to become a Hospice Medical Director, a position he has held since 2007. Dr. Schrier has extensive experience with non-medical aspects of practice – including staffing, scheduling, marketing, advertising, education, and community involvement. Dr. Schrier has a lifelong passion for animals (especially dogs), art, philanthropy, equestrian competition, physical fitness/nutrition, gardening, and community service.
Consulting Psychiatrist
 Dr. Martin attended Oberlin College (BA Biology) and Georgetown University School of Medicine. Her residency in Psychiatry was completed there, as well. She has been certified by the joint Board of Psychiatry and Neurology as a psychiatrist since 1983. She went on to complete training in psychoanalysis and she has been in the practice of general psychiatry in this area for the last thirty-plus years. Drawn to the intersection of Psychiatry and Medicine, she has always had a special interest in working with people living with chronic medical illnesses, as well as an abiding interest in hospice and end-of-life care.
Dr. Martin attended Oberlin College (BA Biology) and Georgetown University School of Medicine. Her residency in Psychiatry was completed there, as well. She has been certified by the joint Board of Psychiatry and Neurology as a psychiatrist since 1983. She went on to complete training in psychoanalysis and she has been in the practice of general psychiatry in this area for the last thirty-plus years. Drawn to the intersection of Psychiatry and Medicine, she has always had a special interest in working with people living with chronic medical illnesses, as well as an abiding interest in hospice and end-of-life care.
Nurse Practitioners
 Yiesak Asfaw is a DNP, APRN, and Board -Certified Family Nurse Practitioner. He completed his Doctor of Nurse Practice Degree at Grand Canyon University Phoenix, Arizona. Before his doctoral degree, he earned a Master of Science in Nursing with a postmaster Certificate Family Nurse Practitioner from Bowie State University. As a family nurse practitioner, he held a national certification with the American Academy of Nurse Practitioner (AANP). He also earned a Bachelor of Science in Nursing from the University of District of Columbia, Washington, D.C.
Yiesak Asfaw is a DNP, APRN, and Board -Certified Family Nurse Practitioner. He completed his Doctor of Nurse Practice Degree at Grand Canyon University Phoenix, Arizona. Before his doctoral degree, he earned a Master of Science in Nursing with a postmaster Certificate Family Nurse Practitioner from Bowie State University. As a family nurse practitioner, he held a national certification with the American Academy of Nurse Practitioner (AANP). He also earned a Bachelor of Science in Nursing from the University of District of Columbia, Washington, D.C.
After earning a postmaster Certificate Family Nurse Practitioner, he worked for almost eight years as a provider in various settings – including as a primary care provider, urgent care, long-term care, rehabilitation, and currently at Montgomery Hospice and Prince George’s Hospice as part of the medical team. He enjoyed 15 years fulfilling years of nursing experience, including in the Emergency Department, trauma, infection disease, and medical-surgical care.
His experience as a bedside critical care nurse and becoming advanced practice helped him to utilize evidence-based practice guidelines that have shaped his approach to work and providing patient and family centered advanced practice care.
 NP Denton obtained her Family Nurse Practitioner degree from Georgetown University. She has extensive experience in hospice, primary care, and hematology-oncology. She grew up in Poland. Her culturally and ethnically diverse background allows her to relate effectively to the diverse population in the metropolitan Washington DC area. Her compassionate, open-minded, and enthusiastic approach to patient care helps her develop long lasting and trusting relationships with her patients and their families.
NP Denton obtained her Family Nurse Practitioner degree from Georgetown University. She has extensive experience in hospice, primary care, and hematology-oncology. She grew up in Poland. Her culturally and ethnically diverse background allows her to relate effectively to the diverse population in the metropolitan Washington DC area. Her compassionate, open-minded, and enthusiastic approach to patient care helps her develop long lasting and trusting relationships with her patients and their families.
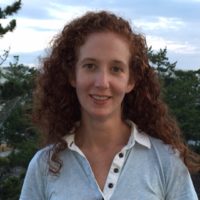
 Meghan earned her BSN from Villanova University and her MSN from the University of Pennsylvania. She is an ANCC board certified Family Nurse Practitioner and has experience caring for patients of all ages. Meghan joined the Montgomery Hospice, Inc. team in 2019 recognizing the privilege to meet and support patients, young and old, and their families, alongside an interdisciplinary team, at end of life. She lives in Montgomery County, down the street from her parents and childhood home, with her husband, three children, and puppy. She enjoys spending time outdoors with family and friends, running, and reading.
Meghan earned her BSN from Villanova University and her MSN from the University of Pennsylvania. She is an ANCC board certified Family Nurse Practitioner and has experience caring for patients of all ages. Meghan joined the Montgomery Hospice, Inc. team in 2019 recognizing the privilege to meet and support patients, young and old, and their families, alongside an interdisciplinary team, at end of life. She lives in Montgomery County, down the street from her parents and childhood home, with her husband, three children, and puppy. She enjoys spending time outdoors with family and friends, running, and reading.
 Jennifer Jordan, MS, FNP-BC received her Master’s and Bachelor’s degrees in nursing from University of Maryland and Johns Hopkins University respectively and is an ANCC board-certified family nurse practitioner. She additionally has a BA in physics and environmental sciences from University of California, Berkeley and in an earlier career worked as a climate change and environmental researcher. Ms. Jordan has served as a nurse practitioner at Montgomery Hospice since 2011. Prior to joining hospice, Ms. Jordan worked alongside a family practice physician for a decade seeing both adult and pediatric patients. As an RN, she worked in the late 1990s at Georgetown University Hospital and George Washington University Hospital in the emergency departments and on medical surgical units. She spent three months serving as the staff nurse at a rural orphanage in Nepal in 1997. Professionally, Ms. Jordan divides her time between hospice and teaching mindfulness meditation. For nearly two decades, she has led mindfulness trainings for groups and individuals across the lifespan. She is Family Program Director at Insight Meditation Community of Washington, teaches mindfulness in schools with Minds, Inc, is a senior mentor for the online Power of Awareness course, and is a certified Level 3 Reiki Practitioner. She has extensive training in a variety of contemplative and healing modalities.
Jennifer Jordan, MS, FNP-BC received her Master’s and Bachelor’s degrees in nursing from University of Maryland and Johns Hopkins University respectively and is an ANCC board-certified family nurse practitioner. She additionally has a BA in physics and environmental sciences from University of California, Berkeley and in an earlier career worked as a climate change and environmental researcher. Ms. Jordan has served as a nurse practitioner at Montgomery Hospice since 2011. Prior to joining hospice, Ms. Jordan worked alongside a family practice physician for a decade seeing both adult and pediatric patients. As an RN, she worked in the late 1990s at Georgetown University Hospital and George Washington University Hospital in the emergency departments and on medical surgical units. She spent three months serving as the staff nurse at a rural orphanage in Nepal in 1997. Professionally, Ms. Jordan divides her time between hospice and teaching mindfulness meditation. For nearly two decades, she has led mindfulness trainings for groups and individuals across the lifespan. She is Family Program Director at Insight Meditation Community of Washington, teaches mindfulness in schools with Minds, Inc, is a senior mentor for the online Power of Awareness course, and is a certified Level 3 Reiki Practitioner. She has extensive training in a variety of contemplative and healing modalities.
 Ellen Owusu is a board-certified family nurse practitioner and received her master’s in nursing degree from Walden University. She has experience working at the oncology unit at Suburban Hospital and worked in the cardiology unit at Providence Hospital as a registered nurse. She continues to further her nursing training as a nurse practitioner at Montgomery Hospice and Prince George’s Hospice.
Ellen Owusu is a board-certified family nurse practitioner and received her master’s in nursing degree from Walden University. She has experience working at the oncology unit at Suburban Hospital and worked in the cardiology unit at Providence Hospital as a registered nurse. She continues to further her nursing training as a nurse practitioner at Montgomery Hospice and Prince George’s Hospice.
 Nicky Pilgrim is a board-certified adult-geriatric Nurse Practitioner who specializes in providing Palliative care and Hospice care to patients with advanced, life limiting, chronic illnesses. Focusing on quality-of-life improvement by establishing a plan of care that includes guidance on disease trajectory overtime, symptom evaluation and management, and advance care planning. Nicky considers it a privilege to support patients and families who are navigating the challenges of serious illness and symptoms associated with advanced and end-of life disease progression.
Nicky Pilgrim is a board-certified adult-geriatric Nurse Practitioner who specializes in providing Palliative care and Hospice care to patients with advanced, life limiting, chronic illnesses. Focusing on quality-of-life improvement by establishing a plan of care that includes guidance on disease trajectory overtime, symptom evaluation and management, and advance care planning. Nicky considers it a privilege to support patients and families who are navigating the challenges of serious illness and symptoms associated with advanced and end-of life disease progression.
 Melanie Reynolds is committed to providing compassionate, high quality, Community Based Healthcare to patients with serious illnesses. Ms. Reynolds is an Adult Nurse Practitioner with certifications in Oncology and Hospice and Palliative Care. She is a graduate of Eastern Mennonite University and the University of Maryland at Baltimore.
Melanie Reynolds is committed to providing compassionate, high quality, Community Based Healthcare to patients with serious illnesses. Ms. Reynolds is an Adult Nurse Practitioner with certifications in Oncology and Hospice and Palliative Care. She is a graduate of Eastern Mennonite University and the University of Maryland at Baltimore.
 Marisa Tamari received a B.S. in nursing from The Catholic University of America and a M.S. in nursing from Georgetown University. She is an ANCC board certified family nurse practitioner. Most of her career has been in research settings–first at the Georgetown University Medical Center, where she worked primarily with HIV/AIDS patients and, later, at the National Institutes of Health, where her work focused on patients undergoing bone marrow transplantation. These professional experiences led her to develop an enduring interest and commitment to compassionate end-of-life care. In 2015 she completed training in Dignity Therapy at the Manitoba Palliative Care Research Unit in Winnipeg, Canada and decided to redirect her practice toward providing care in the final phase of life. As a child whose parents came from different cultural traditions, Ms. Tamari cultivated an interest in the power of personal stories as a therapeutic tool. She is a trained Story Corps facilitator in their Legacy program and is the proprietor of Keepsake Conversations, LLC, a legacy document service based on the Dignity Therapy protocol. Through this service, individuals with life-threatening illness or life-limiting conditions create an enduring document derived from a review of their values and formative life experience.
Marisa Tamari received a B.S. in nursing from The Catholic University of America and a M.S. in nursing from Georgetown University. She is an ANCC board certified family nurse practitioner. Most of her career has been in research settings–first at the Georgetown University Medical Center, where she worked primarily with HIV/AIDS patients and, later, at the National Institutes of Health, where her work focused on patients undergoing bone marrow transplantation. These professional experiences led her to develop an enduring interest and commitment to compassionate end-of-life care. In 2015 she completed training in Dignity Therapy at the Manitoba Palliative Care Research Unit in Winnipeg, Canada and decided to redirect her practice toward providing care in the final phase of life. As a child whose parents came from different cultural traditions, Ms. Tamari cultivated an interest in the power of personal stories as a therapeutic tool. She is a trained Story Corps facilitator in their Legacy program and is the proprietor of Keepsake Conversations, LLC, a legacy document service based on the Dignity Therapy protocol. Through this service, individuals with life-threatening illness or life-limiting conditions create an enduring document derived from a review of their values and formative life experience.
VP of QAPI
Performance Improvement, Risk Management & Health Information
 Cornelia Stronge is a registered nurse with 23 years of nursing experience, nine of which have been in hospice clinical management. She obtained her BSN degree from City University in London. She is a Certified Hospice and Palliative Nurse (CHPN) and is currently pursuing a master’s degree in Healthcare Administration.
Cornelia Stronge is a registered nurse with 23 years of nursing experience, nine of which have been in hospice clinical management. She obtained her BSN degree from City University in London. She is a Certified Hospice and Palliative Nurse (CHPN) and is currently pursuing a master’s degree in Healthcare Administration.
Cornelia’s main clinical focus has been medical, surgical and community health care, as well as end- of-life care. During her 11 years at Montgomery Hospice and Prince George’s Hospice, she has developed and fostered good working relationships with healthcare partners and actively participates in community education.
Board Leadership
Board of Directors
Life Directors
- Paul Alpuche
- Edward Hall Asher
- Beryl Feinberg
- Suzanne Firstenberg
- Arnold Kohn
- Catherine S. Leggett
- Brian McCagh
- Margaret McCaig
- Michael McCarthy
- Deborah Neipris
- Richard Pettit
- Karen Schaeffer

















